Abstract
This article presents a case report of a patient with Angle Class III malocclusion and total crossbite, nasal breathing, treated in 11 months with the GUIA PAM III (Postero Anterior Marinho’s) appliance. Early treatment, initiated at 6 years and 8 months repositioned and controlled mandibular growth and corrected the crossbite. Cephalometric measurements taken before and after treatment were used to evaluate the changes resulting from the use of the PAM III appliance proved effective in both stimulating maxillary growth and in increasing maxillary length. According to the results obtained in the initial and final cephalometric measurements, we were able to observe significant changes such as the cephalometric values SNA, which was 84.54° and changed to 86.46°, and 1/.NA, which was 7.72° and changed to 17.14°.
1. Introduction
In 1968, Professor Alfeu V. Marinho Filho conceived the Jaw Functional orthopedic appliance Marinho's Posterior Anterior Guide (GUIA PAM) in Brazil. It is used to correct skeletal Angle Class I, II, and III malocclusions that require stimulating or repositioning the mandible [1].
According to Wang, the PAM Guide causes little discomfort to the patient. With its smaller volume and progressive activations, it achieves excellent results in a short treatment period [2].
Although Class III malocclusion is less frequent in dental clinics, its early interception is crucial to prevent the worsening of the condition, bone compromise, and impact on the patient's self-esteem. Early treatment of Class III malocclusion, which includes anterior crossbite, using functional maxillary orthopedic appliances is crucial to prevent the worsening of the occlusion. Additionally, it helps to preserve the patient's bone profile and maintain self-esteem, preventing future problems such as tooth extractions and, in extreme cases, orthognathic surgery.
Skeletal anterior crossbite is linked to a Class III basal pattern, characterized by maxillary retrognathia, mandibular prognathism, or a combination of both. Functional anterior crossbite, also known as pseudo-Class III, occurs when there is interference in the dental occlusion, forcing the mandible to deviate to reach maximum intercuspation [3].
After diagnosis, anterior crossbite correction should be performed as soon as possible, as this type of malocclusion does not correct itself spontaneously and tends to worsen. The worsening of this malocclusion can result in traumatic occlusion, irregular tooth wear, periodontal alterations such as gingival recession and mobility in the lower incisors, temporomandibular dysfunction, as well as aesthetic damage, have been associated with the worsening of the malocclusion [4, 5].
This study presents a successful case of treatment of a patient with Class III malocclusion using the functional maxillary orthopedic appliance PAM III GUIDE, highlighting its simplicity, comfort, and freedom of mandibular movement [7].
2. Clinical case description
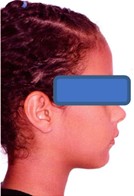
The clinical case presented refers to a patient, J.S.M.B., who was treated at the private in Natal, RN, Brazil. The female patient, of Caucasian ethnicity, began treatment at the age of 6 years and 8 months, accompanied by her legal guardian. She presented good oral health, mixed dentition, Angle Class III malocclusion with a total crossbite, passive lip sealing, and nasal breathing.
The initial orthodontic documentation was performed on August 11, 2021, and the appliance was installed on January 10, 2022. The patient was instructed to wear the device for 20 hours a day, removing it to eat and brush his teeth [7]. At the end of the active phase of treatment, on December 12, 2022, new orthodontic documentation was performed, at which time the patient was instructed to use the GUIA PAM III appliance only during the nighttime as a retention appliance, with follow-up appointments every 4 months. Because the crossbite correction and occlusion are stable and functional, with the treatment in the retention phase, the patient does not need to visit the office monthly. The results of the two cephalometric analyses, initial and final of the active phase of treatment, are presented in Table 1, revealing positive results using the GUIA PAM III functional orthopedic appliance.
Fig. 1Initial orthodontic documentation: a) extraoral smiling photograph; b) frontal extraoral photograph; c) lateral extraoral photograph; d) lateral cephalometric teleradiograph; e) intraoral photograph of the right side; f) frontal intraoral photograph; g) intraoral photograph of the left side; h) panoramic radiograph

a)

b)

c)

d)

e)

f)

g)
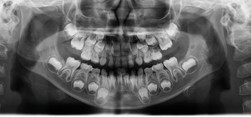
h)
3. Treatment
The PAM III guide appliance is part of the PAM guide technique. It is indicated for the correction of Angle Class III malocclusion, including anterior or total crossbite, promoting mandibular repositioning and anterior maxillary advancement. The images below show the PAM III guide appliance in position in the patient's mouth and on the plaster model, dated June 3, 2022.
Treatment progressed with monthly maintenance and arch activations, counting on the patient's collaboration with respect to use. Below, we present extraoral, intraoral photographs, and radiographs taken on December 12, 2022. The patient continues to use the same appliance as retention, with the addition of a central expander activated for three months as can be seen in figure number 3. We will evaluate the need for fixed appliance installation in the future.
The device is made in habitual occlusion and the “constructive bite” is made by activating the archwire, positioning the jaw in the posterior region, creating a lever, stimulating the maxilla using the reaction of the archwire force. In other words, the action of the force that is applied to the jaw and the reaction is the stimulation of the maxilla. The Hawley archwire was added only to generate stability to avoid the tilting movement when the patient closes the mouth, but it is not mandatory. The helicoid in the posterior curve of the active archwire of the GUIA PAM must be close to the vestibular surface of the posterior teeth so as not to irritate the patient's buccal mucosa. This helicoid has the function of activating the device and preventing the archwire from breaking.
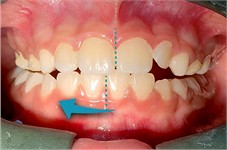
Fig. 2Appliance Photographs – June 3, 2022: a) right-side intraoral photograph; b) frontal intraoral photograph; c) left-side intraoral photograph; d) photograph of the appliance placed on the study model

a)

b)

c)

d)
We can observe in the analysis of the cephalometric measurements that the lower incisors were at the beginning of the treatment with vestibular inclination. In order to correct this inclination during the treatment, a lower brace was not installed. If it were necessary to maintain the inclination of the lower incisors, it would be necessary to leave the arch of the upper brace touching the cervical region of the lower teeth, without touching the incisors, and/or to make a removable lower plate with the resin touching the lingual surface of the lower incisors. In this way, the lower incisors would maintain the original inclination without movement.
Fig. 3Orthodontic records – December 12, 2022: a) frontal extraoral photograph; b) smiling extraoral photograph; c) right lateral extraoral photograph; d) right intraoral photograph; e) frontal intraoral photograph; f) left intraoral photograph; g) panoramic radiograph; h) lateral cephalometric radiograph

a)

b)
c)

d)

e)

f)

g)

h)
As can be observed in Fig. 3(a, c), the patient’s profile has significantly changed. The patient’s profile, previously classified as Class III, now exhibits a more aesthetically pleasing Class I pattern. In Fig. 3(d, f), we note the mandible repositioning, with the right and left posterior teeth in a cusp-to-cusp relationship, indicating considerable improvement in occlusion. Furthermore, Fig. 3(e) demonstrates the correction of the anterior crossbite, restoring the patient's masticatory function.
Crossbite interferes with chewing efficiency, making it difficult to properly grind food. Correction of crossbite allows for functional occlusion, facilitating bilateral chewing and making chewing more efficient, which contributes to better digestion and nutrient absorption. Early correction of patients during the growth phase can positively influence the skeletal pattern, avoiding or minimizing the need for more invasive interventions in the future, such as orthognathic surgery. By addressing the skeletal foundations and promoting functional occlusion, OFM seeks to establish a more stable correction in the long term, reducing the likelihood of relapse compared to purely dental treatments.
Between December 2022 and May 5, 2023, the patient used the appliance only at night as retention. In May 2023, a new treatment plan was developed, and another identical appliance was made with the addition of a central expander to complete the correction of the posterior crossbite and expand the upper arch. The expander was activated ⅛ of a turn by the patient twice a week until July 24, 2023. After the posterior teeth were no longer in crossbite, the patient was instructed to discontinue the activations and use the appliance only at night.
Fig. 4Photographs taken on February 10, 2025, intraoral views with the appliance in place and without the appliance: a) photograph with the appliance in place, right side view; b) photograph with the appliance in place, left side view; c) frontal intraoral photograph with the appliance in place; d) intraoral photograph of the appliance with an occlusal view showing the central expander; e) intraoral photograph without the appliance, right side view; f) frontal intraoral photograph without the appliance; g) intraoral photograph without the appliance, left side view

a)

b)

c)

d)

e)

f)

g)
Fig. 5Functional intraoral photographs with mandibular movements: a) intraoral photograph with protrusive movement; b) intraoral photograph with right lateral mandibular movement; c) intraoral photograph with left lateral mandibular movement

a)
b)

c)
The photographs in Figs. 4 and 5, taken on February 10, 2025, show the patient’s condition with and without the appliance in place and functional mandibular movements. The patient will use the appliance as retention for an additional 3 months, after which its use will be discontinued.
We observed that the patient exhibits lateral and protrusive movements within normal limits. The protrusive movement, with contact occurring on both central incisors. The left and right lateral movements also appear favorable for functional occlusion, with no canine guidance due to their stage of eruption.
The patient’s bone and muscle development, during the growth phase, progressed satisfactorily with the use of the Guia Pam III appliance, as expected and observed in the cephalometric data. This included maxillary development with increased SNA values, a slight decrease in SNB, and a significant increase between the points observed in ANB, due to the orthopedic effect promoted by the appliance.
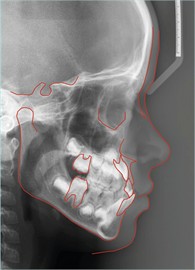
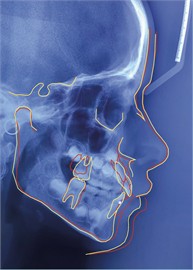
Fig. 6Cephalometric analyses: a) initial cephalometric analysis of the patient, performed in August 2021 traced in the color red; b) cephalometric analysis performed in December 2022 cephalometric analysis was performed in December 2022 and traced in yellow. Superimposition of the two cephalometric analyses
a)

b)
c)
In the images above, displayed in Fig. 6, we observe the superimposition of serial cephalometric tracings. This allows for monitoring of craniofacial development and evaluation of the effectiveness of treatment performed with the Guia PAM III appliance, making it possible to compare dental and skeletal changes.
The results showed that the treatment promoted significant changes in craniofacial structures, with a change in mandibular posture, increased maxillary projection, correction of the relationship between the bony bases, and improved dental occlusion.
4. Discussion
The Guia PAM appliance is a functional orthopedic maxillary appliance designed to correct skeletal and dental malocclusions, improving the anteroposterior relationship of the dental arches.
Cephalometric measurements taken before and after treatment were used to evaluate the changes resulting from the use of the PAM III appliance, as presented in Table 1. The SNA angle increased by 1.92°, while the ANB angle, which indicates the relationship between the maxilla and mandible, increased by 2.89°, representing an improvement in the anteroposterior relationship of the bony bases.
Table 1Results of the initial and final cephalometric analyses of the active phase of treatment, demonstrating the benefits of treatment with Guia PAM III appliance
Cephalometric measurement | Initial doc. 11 / august / 2021 | Final doc. 12 / December / 2022 | Default value |
SNA | 84,54° | 86,46° | 82° |
SNB | 82,80° | 81,83° | 80° |
ANB | 1,73° | 4,62° | 2° |
SND | 78,67° | 77,55° | 76° |
1/.NA | 7,72° | 17,14° | 22° |
/1.NB | 34,03° | 24,48° | 25° |
1/.NS | 92,27° | 103,61° | 103° |
FMA | 22,91° | 24,62° | 25° |
(Sn-Gn).(Go-Me) | 32,16° | 33,29° | 32° |
Maxillary length (Enp-Ena) | 49,04 mm | 50,24 mm | 47 mm |
Mandibularlength(Bpc-Pog-Go-Me) | 94,87 mm | 97,38 mm | 103 mm |
Mandibularramuslength(Co-Go) | 51,27 mm | 46,90 mm | 53 mm |
Regarding the Enp-Ena measurement, which indicates the length of the maxilla, an increase of 1.20 mm was observed, consistent with the findings of Marinho7, 1998, in the Co-A measurement obtained in a sample of 31 female patients.
Increases were also observed in the angular values (Sn-Gn).(Go-Me) and FMA, which reflect the inclination of the mandibular plane in relation to the cranial base. There was an increase of 1.13° in (Sn-Gn).(Go-Me) and 1.71° in FMA, indicating an increase in anterior facial height and better positioning of the mandible.
Regarding incisor inclination, the upper incisors showed vestibular inclination, with an increase in the 1/NA angle from 7.72° to 17.14°, approaching the ideal pattern. The 1/NS angle also increased, from 92.27° to 103.61°, reaching the standard value of 103°, which confirms the vestibular inclination of the upper incisors. In contrast, the lower incisors showed a reduction in the 1/NB angle, from 34.03° to 24.48°, indicating a significant lingual inclination, approaching the ideal standard value of 25°.
These changes in cephalometric variables contributed to the correction of Class III malocclusion and improved facial aesthetics in the patients.
5. Conclusions
In conclusion, this case study successfully demonstrates the effectiveness of the GUIA PAM III functional orthopedic appliance in treating a Class III malocclusion with anterior crossbite in a young patient. The appliance's design, emphasizing patient comfort and mandibular freedom, facilitated significant skeletal and dental improvements, as evidenced by the positive changes in cephalometric measurements.
Notably, the increase in the ANB angle and the favorable repositioning of the mandible and maxillary advancement highlight the appliance's capacity to address the underlying skeletal discrepancies. Furthermore, the correction of the anterior crossbite and the establishment of a more functional occlusion underscore the clinical benefits of early intervention with the GUIA PAM III.
The long-term stability achieved during the retention phase suggests the potential for lasting positive outcomes, minimizing the need for more invasive future interventions. This case reinforces the value of the GUIA PAM III as a simple, comfortable, and effective tool in the functional orthopedic correction of Class III malocclusions in growing patients.
Additionally, balance was achieved in the patient's stomatognathic system. Both orthodontic records were obtained at the same dental radiology clinic (IORN) in Natal/RN, using the same radiography equipment, processed with the same software and computer equipment (the x-ray device was promax type 2d scara 3 gui software 3.6.1.0.r. promax and the software used for cephalometric analysis was).
References
-
R. R. Marinho et al., “Guide PAM a new orthodontic and orthopedic appliance to treat Angle Classe II and III malocclusions,” (in Portuguese), Brazilian Journal of Orthodontics and Maxillary Orthopedics, Vol. 3, No. 18, pp. 24–35, 1998.
-
Wang and J. L. M., “Cephalometric Evaluation of Postero-Anterior Mandibular Positioning Using NAP, ANB, H-NB, Wits, A’B’-ABC-M’S, SND, and Co-Gn Measurements in Both Sexes Before and After the Use of the Class II Marinho’s Postero-Anterior Guide (PAM),” Paulista School of Dentistry, 1997.
-
S. Bayrak and E. S. Tunc, “Treatment of anterior dental crossbite using bonded resin-composite slopes: case reports,” European Journal of Dentistry, Vol. 2, No. 4, pp. 303–306, Oct. 2019, https://doi.org/10.1055/s-0039-1697397
-
L. M. A. Seabra, N. L. F. Fernandes, R. M. Lira, D. G. Souto, L. P. Oliveira, and D. T. Medina, “Anterior crossbite: treatment possibilities in deciduous and mixed dentition,” (in Portuguese), Revista Naval de Odontologia, Vol. 46, No. 1, pp. 59–68, Jan. 2019, https://doi.org/10.29327/25149.46.1-10
-
V. G. Francisco de Assis, S. Gribel, and A. Mamede, “Anterior crossbite treatment using functional orthopedic appliance: a case report,” Jaw Functional Orthopedics and Craniofacial Growth, Vol. 3, No. 1, pp. 19–31, Jun. 2023, https://doi.org/10.21595/jfocg.2023.23333
-
E. A. S. Serrano et al., Orthodontics and Orthopedics. (in Portuguese), Brasil: Nova Odessa, 2016.
-
R. R. Marinho, “Comparison of cephalometric measurements obtained from lateral cephalometric radiographs of the head before and after orthodontic treatment using the Marinho’s Postero-Anterior Orthopedic Guide for the correction of Angle Class II and Class III malocclusions,” (in Portuguese), Faculty of Dentistry, UNESP, 1998.
-
H. Mitani and H. Fukazawa, “Effects of chincap force on the timing and amount of mandibular growth associated with anterior reversed occlusion (Class III malocclusion) during puberty,” American Journal of Orthodontics and Dentofacial Orthopedics, Vol. 90, No. 6, pp. 454–463, Dec. 1986, https://doi.org/10.1016/0889-5406(86)90105-8
-
P. D. Wendell, R. Nanda, and S. Nakamura, “The effects of chin cup therapy on the mandible: A longitudinal study,” American Journal of Orthodontics, Vol. 87, No. 4, pp. 265–274, Apr. 1985, https://doi.org/10.1016/0002-9416(85)90001-6
About this article
The authors have not disclosed any funding.
To the scientist and doctor ALFEU VITELLI MARINHO FILHO in memoriam.
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
Rodolfo Ribeiro Marinho: conceptualization, data curation, project administration, supervision, visualization, writing-original draft preparation, writing-review and editing. Leon de Freitas Daghlian: conceptualization, data curation, investigation, methodology, project administration, resources, writing-original draft preparation, writing-review and editing. Fabiola Rodrigues Marinho: conceptualization, data curation, writing-original draft preparation, writing-review and editing. Vinicius Rodrigues Marinho: conceptualization, data curation, software, writing-original draft preparation, writing-review and editing.
The authors declare that they have no conflict of interest.
The research met all applicable standards for the ethics of experimentation. According to resolution No. 466, there is no need for approval of the research by the ethics committee. Participants provided written informed consent prior to the study.
