Abstract
Diagnosis and treatment of mesiocclusion in the deciduous denture can provide balance for the development of occlusion, function, and aesthetics during craniofacial growth and development [1-4]. Jaw Functional Orthopedic (JFO) intervention was performed starting in the deciduous dentition, using the principles of Neuro Occlusal Rehabilitation (NOR) and use of functional orthopedic devices with subsequent follow-up, in two children diagnosed with distinct skeletal Classe III malocclusion. The treatment provided harmonious growth and development between the bone bases of the jaws, compatibility between the middle and lower thirds of the face, improvement in the lateral cephalometric profile, with alteration in the gonial angle, especially in the patient who started treatment at 3 years old of age; thus, avoiding future functional, aesthetic and skeletal complications for the craniofacial complex.
1. Introduction
There are different schools of thought regarding the timing of treatment for the management of class III skeletal malocclusion. We present here two clinical case reports of patients diagnosed with different mesiocclusions. The different diagnosis was made based on lateral profile cephalometry, clinical examination with intraoral photos, and examination of masticatory and respiratory functions. Class III pseudo malocclusion was identified based on its functional origin, presenting an anterior crossbite, negative sagittal step between the maxilla and mandible and dental and facial relationships similar to those observed in Class III. The true Class III was identified based on specific skeletal characteristics, maxillary retrusion, mandibular prognathism, open gonial angle. The treatment of these two malocclusions was carried out with JFO during the period of primary dentition and monitoring during growth and craniofacial development. L.D.C., class III patient with a tendency to vertical growth of the mandible and M.E.C.A., pseudo-class III patient. With the functional orthopedic treatment of the jaws, it was possible to provide harmonious growth and development between the bone bases of the jaws and avoid functional, aesthetic and skeletal complications for the craniofacial complex.
2. Methodology
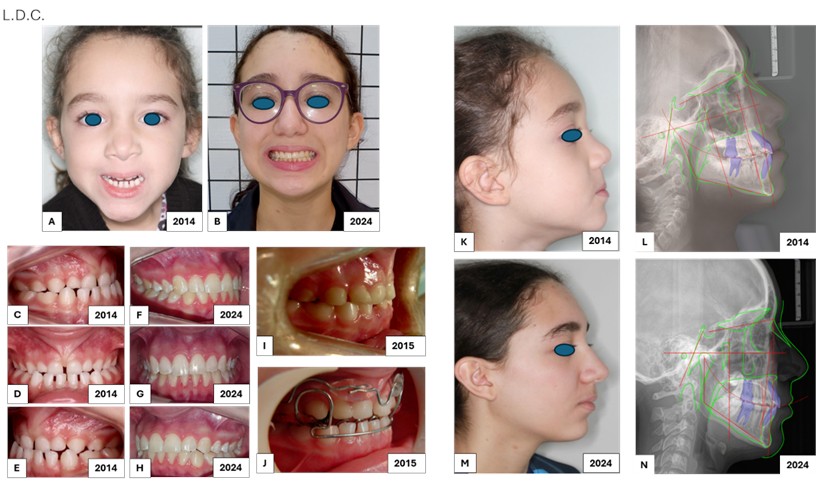
JFO treatment was performed in two children, starting on deciduous dentition, diagnosed with different skeletal class III characteristics, true Class III and pseudo Class III, mesiocclusion, leptognaths. L.D.C., Fig. 1, started treatment in July 2014, at 4 years and eight months of age, skeletal class III, tendency to vertical growth of the mandible, excessive curvature of the cervical spine, hypertrophic labial frenum and severe growth deficiency in the anterior region of the maxilla. Treatment was conducted for a period of 18 months, with monthly returns. Initially, NOR was performed with selective wear grinding, occlusal adjustment and addition of resin on the palatal and incisal surface of the upper deciduous incisors, with a 35-degree inclination, promoting the uncrossing of the anterior crossbite [3]. Change in therapeutic posture between the mandible and maxilla with two devices, first one, Planas’s Special Indirect Tracks (PIPE) with Eschler’s Arch and Upper Lip Shield in the premaxilla region, favoring new bone formation in this region and the eruption of the upper incisors in the correct position. Uncrossing of the anterior crossbite was achieved in September 2015, but there was still a need to expand the arches, prioritizing the maintenance of the change in mandibular posture achieved, we used a second devise, Planas’s Indirect Track Composite Compound (PIPC), with lower dorsal arch, telescopic tube in the maxillary acrylic and Äeschler Arch. This case was followed during the next 8 years bimonthly and then semi-annually. M.E.C.A., Fig. 2, started treatment in July 2019, at 3 years and 11 months of age, pseudo class III, anterior crossbite, superior airways with reduced space, alteration in the eruption corridor of the upper incisors, and maxillary growth deficiency. The treatment instituted, for a period of 20 months, also with NOR, selective wear grinding, occlusal adjustment and addition of resin on the palatal and incisal surface of the upper deciduous incisors, in 35-degree inclination, promoting the uncrossing of the anterior crossbite [3]. PIPC, with Äeschler’s Arch and subsequent follow-up bimonthly and now biannual, for 3 years. Currently, the two patients continue to undergo semiannual evaluations.
Fig. 1Patient L.D.C.: a) frontal extraoral photo, 4 years and 8 months, 2014; b) frontal extraoral photo, 15 years old, 2024; c) right lateral intraoral photo, severe maxillary growth deficiency 2014; d) frontal intraoral photo; e) left lateral intraoral photo; f) right lateral intraoral photo, harmonic relationship between the jaws, 2024; g) frontal intraoral photo; h) left lateral intraoral photo; i) adaptation of resin in the palatal region of the upper incisors with an inclination of 35 degrees, indirectly, performed first on the working model and transferred to the tooth, these 35 degrees are measured according to the long axis of the tooth crown and allow the lower incisors to be positioned correctly in relation to the upper incisors, reestablishing the correct DA, Determined Area.; j) Planas’ Special Flat Indirect Tracks (PIPE) with Äeschler Arch and Upper Lip Shield; k) extraoral photo in right side profile; l) initial lateral teleradiographs, m) extraoral photo in right lateral profile; n) final lateral radiograph
3. Findings
The JFO intervention, during the deciduous dentition in the patient L.D.C., provided a significant and rapid growth response in the dental arches, spatially in three dimensions, transverse, vertical and sagittal, mainly in the anterior region of the maxilla, since the maxilla grows steadily until 5 years of age, when 85 % of its size is reached [5]. By changing the therapeutic posture, mandibular growth was redirected towards a harmonious relationship with the maxilla, confirmed by photos and radiographic analysis examinations. By lateral profile cephalometry, comparing the initial results and during the monitoring of the treatments, we were able to observe improvements in the dental skeletal analyses, in the angular analyses of the skeletal profile as well as in the linear measurements evaluated. It was observed that JFO and NOR treatment in patient M.E.C.A. promoted the uncrossing of the anterior crossbite and the posterior crossbite, releasing the growth of the maxilla and mandible, redirecting both to a better position, especially in this patient who started treatment at 3 years of age, which initially presented a pseudo Class III.
Fig. 2Patient M.E.C.A.: A) frontal extraoral photo, 3 years and 11 months, 2019; B) frontal extraoral photo, 9 years old, 2024; C) right lateral intraoral photo, maxillary growth deficiency; D) frontal intraoral photo; E) left lateral intraoral photo; F) right lateral intraoral photo, harmonic relationship between the jaws; G) frontal intraoral photo; H) left lateral intraoral photo; I) left lateral intraoral photo; J) adaptation of resin in the palatal region of the upper incisors with an inclination of 35 degrees, indirectly, performed first on the working model and transferred to the tooth, these 35 degrees are measured according to the long axis of the tooth crown and allow the lower incisors to be positioned correctly in relation to the upper incisors, reestablishing the correct DA, Determined Area.; K) extraoral photo in right side profile; L) initial teleradiography in the right lateral norm; M) extraoral photo in right lateral profile; N) final radiograph in right lateral rule

4. Discussion
Class III malocclusion has a lower prevalence among occlusions, but has a high severity, unfavorable prognosis, greater aesthetic impairment and great need for treatment from the deciduous dentition, which can negatively influence the important and active period of craniofacial growth and development in the first years of life, also considering the negative influence on the quality of life of the patient who has mandibular prognathism with anterior crossbite [1, 6, 7]. Marie-Josèphe Deshayes reaffirms, in her research, that the best time to treat facial asymmetries with the possibility of correcting them and avoiding recurrence is during the deciduous dentition phase, before the first permanent molars enter occlusion [8]. F. Remy, in morphometric studies of the mandible, reports that mandible growth reaches its highest rate during the first 5 years of postnatal life [9, 10]. The American Academy of Pediatric Dentistry, in its latest update, in 2023, on the management of occlusion in the period of deciduous and mixed dentition, highlights that interventions in Class III malocclusions can provide a more favorable environment for craniofacial growth, improve occlusion, function, and aesthetics, intervening in the characteristic factors that involve this malocclusion [2]. O’ Sullivan E, in anthropometric study of the pediatric mandible allowed the understanding of the development of the growing mandibular shape, demonstrating potential to improve diagnostic accuracy for craniofacial conditions that impact mandibular morphology [5]. Matos GR, in a finite element study, demonstrated the influence of adding resin with a 35-degree inclination, on the palatal and incisal surfaces of the upper incisors, in the primary dentition, promoting the uncrossing of the anterior crossbite [3]. Usman, in a study on age-related changes in maxillary and mandibular growth, identified that constant maxillary growth is observed until 5 years of age, in which 85 % of adult size is reached and minimal changes in maxillary growth are seen after 11 years of age [10]. Planas P and Simões WA, advocate Neuro-occlusal Rehabilitation in the deciduous dentition, which effectively promotes the correction of dental and functional deviations, considering the change in mandibular posture, the better positioning of the condyles in the temporomandibular joints and the reestablishment of the correct masticatory function [11, 12].
5. Conclusions
The precise diagnosis of class III mesiocclusion with distinct characteristics during the important and active period of craniofacial growth and development, in the first years of life, during the primary dentition; associated with clinical and assertive management for JFO treatment of these mesiocclusions, provided a change in therapeutic posture between the maxilla and mandible that adequately stimulated orofacial growth and development between the bone bases of the jaws, improved the lateral cephalometric profile; better compatibility between the middle and lower thirds of the face, opened the upper airways, improved the quality of life of these patients and thus avoided future functional, aesthetic and skeletal complications for the craniofacial complex of this patients.
References
-
P. V. P. Oltramari-Navarro, R. R. Almeida, A. C. C. F. Conti, R. L. Navarro, M. R. Almeida, and L. S.A. F. P. Fernandes, “Early treatment protocol for skeletal class III malocclusion,” Brazilian Dental Journal, Vol. 24, No. 2, pp. 167–173, Apr. 2013, https://doi.org/10.1590/0103-6440201301588
-
“Management of the developing dentition and occlusion in pediatric dentistry,” in The Reference Manual of Pediatric Dentistry, Chicago, Ill.: American Academy of Pediatric Dentistry, 2023, pp. 466–83.
-
G. R. Matos, R. R. Neto, A. J. M. Júnior, and R. B. B. Junior, “Influence of the inclination of the incisal edge of Planas direct tracks on deciduous dentition with anterior crossbite: finite-elements study,” European Journal of Dentistry, Vol. 16, No. 3, pp. 528–535, Nov. 2021, https://doi.org/10.1055/s-0041-1735435
-
A. Usman, A. M. Hegde, R. Shetty, and M. R., “Effectiveness of management of skeletal class III malocclusion during primary, mixed, and permanent dentition period – a literature review,” Journal of Health and Allied Sciences NU, Vol. 13, No. 2, pp. 177–186, Oct. 2022, https://doi.org/10.1055/s-0042-1755351
-
E. O. ’ Sullivan et al., “Growth patterns and shape development of the paediatric mandible – A 3D statistical model,” Bone Reports, Vol. 16, p. 101528, Jun. 2022, https://doi.org/10.1016/j.bonr.2022.101528
-
W. M. Thomson and H. L. Broder, “Oral-health-related quality of life in children and adolescents,” Pediatric Clinics of North America, Vol. 65, No. 5, pp. 1073–1084, Oct. 2018, https://doi.org/10.1016/j.pcl.2018.05.015
-
F. M. T. de Vasconcelos et al., “Impact of primary dentition malocclusion on the oral health-related quality of life in preschoolers,” Progress in Orthodontics, Vol. 22, No. 1, p. 38, Nov. 2021, https://doi.org/10.1186/s40510-021-00384-2
-
E. Jaunet, A. Le Guern, P. Le Tacon, C. Thery-Dumeix, and M. Deshayes, “Uncovering and treating asymmetry before 6 years in our daily clinical practice: Option or obligation? Orthodontics or orthopedics?,” in International Orthodontics, European College of Orthodontics, Mar. 2013.
-
F. Remy et al., “Characterization of the perinatal mandible growth pattern: preliminary results,” Surgical and Radiologic Anatomy, Vol. 40, No. 6, pp. 667–679, Apr. 2018, https://doi.org/10.1007/s00276-018-2030-4
-
F. Remy et al., “Morphometric characterization of the very young child mandibular growth pattern: What happen before and after the deciduous dentition development?,” American Journal of Physical Anthropology, Vol. 170, No. 4, pp. 496–506, Oct. 2019, https://doi.org/10.1002/ajpa.23933
-
Planas P., Reabilitação Neuroclusal. Rio de Janeiro: Medsi, 1997.
-
W. Simões, Ortopedia Funcional Dos Maxilares-Vista Através Da Reabilitação Neuro-Oclusal. 2003.
About this article
The authors declare no funding.
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
Renata Pessini Figueira Cerqueira and Maria Cristina F. Buta-Michel: conceptualization, data curation, formal analysis, investigation, methodology, project administration, resources, software, supervision, validation, visualization, writing – original draft, writing – review and editing.
The authors declare that they have no conflict of interest.
These clinical case reports were obtained approved and received signed consent from the parents responsible for the participating patients. The two treatments were carried out at Dr. Renata Pessini Figueira Cerqueira’s private clinic. The scientific basis and organization for presentation in this magazine was carried out by Dr. Renata Pessini Figueira Cerqueira and Dr. Maria Cristina Ferreira Buta Michel.
